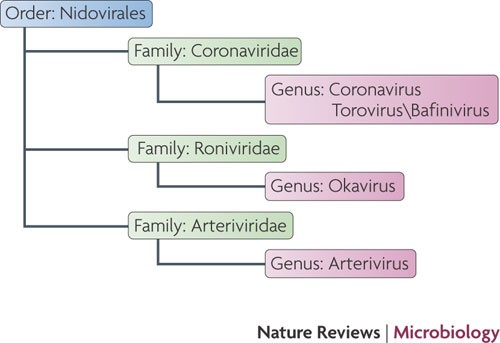
Although coronaviruses were first identified nearly 60 years ago, they only received notoriety in 2003 when one of their members was identified as the aetiological agent of severe acute respiratory syndrome. Previously these viruses were known to be important agents of respiratory and enteric infections of domestic and companion animals and to cause approximately 15% of all cases of the common cold. This Review focuses on recent advances in our understanding of the mechanisms of coronavirus replication, interactions with the host immune response and disease pathogenesis. It also highlights the recent identification of numerous novel coronaviruses and the propensity of this virus family to cross species barriers.
Severe acute respiratory syndrome (SARS)-like bat coronavirus (BtCoV) spread and adapted to wild animals such as the Himalayan palm civet that was sold as food in Chinese wet markets. The virus frequently spread to animal handlers in these markets, but caused minimal or no disease. Further adaptation resulted in strains that replicated efficiently in the human host, caused disease and could spread from person to person.
b | Human coronavirus OC43 (HCoV-OC43) and bovine coronavirus (BCoV) are closely related and it is thought that the virus originated in one species and then crossed species. BCoV has also spread to numerous other animals, such as alpaca and wild ruminants.
c | Feline coronavirus I (FCoV-I) and canine coronavirus I (CCoV-I) are thought to share a common ancestor. CCoV-I underwent recombination with an unknown coronavirus to give rise to canine coronavirus II (CCoV-II). CCoV-II in turn underwent recombination with FCoV-I (in an unknown host) to give rise to feline coronavirus II (FCoV-II). CCoV-II probably also spread to pigs, resulting in transmissible gastroenteritis virus (TGEV).
Coronavirus-mediated diseases
Before the SARS epidemic of 2002–2003, two human coronaviruses, HCoV-OC43 and HCoV-229E, were recognized as important causes of upper respiratory tract infections and were occasionally associated with more severe pulmonary disease in the elderly, newborn and immunocompromised
62. SARS-CoV, unlike HCoV-OC43 and HCoV-229E, causes a severe respiratory disease, and nearly 10% mortality was observed in 2002–2003 (Ref.
1). Notable features of the disease were an apparent worsening of symptoms as the virus was cleared (suggesting the disease had an immunopathological basis), and a lack of contagion until lower respiratory tract symptoms were apparent. This latter feature made control of the epidemic by quarantine feasible, as it simplified identification of infected patients. Unlike HCoV-OC43 and HCoV-229E, SARS-CoV also caused systemic disease, with evidence of infection of the gastrointestinal tract, liver, kidney and brain, among other tissues
63. Although the virus spread primarily via respiratory droplets, infection of the gastrointestinal tract may have facilitated other routes of spread.
The recognition that SARS was caused by a coronavirus intensified the search for other pathogenic coronaviruses associated with human disease, which led to the identification of HCoV-NL63 and HCoV-HKU1. These viruses were isolated from hospitalized patients, either young children with severe respiratory disease (HCoV-NL63)
64,
65 or elderly patients with underlying medical problems (HCoV-HKU1)
65,
66. HCoV-NL63 has infected human populations for centuries, as phylogenetic studies show that it diverged from HCoV-229E nearly 1,000 years ago
67. HCoV-NL63 and HCoV-HKU1 have worldwide distributions and generally cause mild upper respiratory tract diseases, with the exception that HCoV-NL63 is also an aetiological agent of croup
68. HCoV-NL63 can be propagated in tissue culture cells, and an infectious cDNA clone of this virus was recently engineered, facilitating future studies
69. By contrast, HCoV-HKU1 cannot be grown in tissue culture cells, which makes it imperative that an infectious cDNA clone be developed for future studies.
Although the severe disease forming capabilities of human coronaviruses were only recognized because of the SARS epidemic, it was well known that animal coronaviruses could cause life-threatening disease. TGEV, which causes diarrhoea in piglets, infectious bronchitis virus (IBV), a cause of severe upper respiratory tract and kidney disease in chickens, and bovine coronavirus (BCoV), which causes respiratory tract disease and diarrhoea in cattle ('winter dysentery' and 'shipping fever'), are all economically important pathogens. Feline infectious peritonitis virus (FIPV), a virulent feline coronavirus (FCoV), causes an invariably fatal systemic disease in domestic cats and other felines. Unlike most strains of FCoV, which are endemic causes of mild diarrhoea, FIPV arises sporadically, most likely by mutation or deletion in felines persistently infected with enteric strains of FCoV
70, and is macrophage-tropic.
Perhaps the most convincing explanation for FIPV-mediated disease was suggested by the observation that progressive waves of virus replication, lymphopenia and ineffectual T cell responses occurred in feline infectious peritonitis (FIP)
71. In conjunction with previous studies, these results raised the possibility that FIPV infection of macrophages and dendritic cells caused aberrant cytokine and/or chemokine expression and lymphocyte depletion, resulting in enhanced virus loads and, consequently, a fatal outcome. Although this explanation is appealing, additional work is needed to prove its validity. Notably, anti-FIPV antibody-mediated enhancement has been implicated in pathogenesis, but this has been shown only after immunization with S protein expressing vaccines
72; it has not been shown to play a role in a natural feline infection.
Cross-species transmission
A striking feature of the 2002–2003 SARS epidemic was the ability of the SARS-CoV to cross species from Himalayan palm civets (
Paguma larvata), raccoon dogs (
Nyctereutes procyonoides) and Chinese ferret badgers (
Melogale moschata) to infect human populations
73 (
Fig. 5a). Transmission occurred in live animal retail (wet) markets, where animal handlers became infected. In retrospect, it seems that variants of SARS-CoV related to the epidemic strain infected human populations in the wet markets fairly frequently, as is shown by the high seropositivity rate detected in animal handlers who did not develop SARS-like illnesses
73. The epidemic began when a physician who was treating personnel in the wet markets became infected and subsequently infected multiple contacts
This Paper was written in Nature magazine. We had prior knowledge. Also talks about Hydrochlroxine not being affective...
Coronaviruses gained prominence during the SARS outbreaks of 2002–2003, but there are many different coronaviruses that infect humans and animals. Perlman and Netland describe the biology of the coronaviruses, including their replication, host immune response and interspecies transmission.

www.nature.com