Unsurprisingly, it didn’t take long for antivaxxers to try to link COVID-19 vaccines to cancer as well, with attempts beginning even before the FDA granted an emergency use authorization (EUA) for the Pfizer vaccine two years ago. First, they falsely claimed that the mRNA vaccines “permanently alter your DNA” even though basic molecular biology should have told them that mRNA in the vaccine can’t integrate into your genome, and that the mRNA vaccines were “gene therapy, not vaccines” complete with a conspiracy theory about the CDC having supposedly changed the definition of a vaccine to include them. Next came misrepresenting old studies to claim that mRNA causes cancer. More recently, long-time antivax lawyer Thomas Renz got access to the Defense Medical Epidemiology Database (DMED), a database tracking the health of military personnel, and used it to make claims that are, at best erroneous and at worst intentionally misleading, specifically that COVID-19 vaccines have resulted in an epidemic of cancer in military personnel, including a nearly 900% increase in esophageal cancer and a nearly 500% increase in breast and thyroid cancers since before the military imposed its vaccine mandate. As I explained at the time, the claims were incredible on their face just from a scientific plausibility standpoint given that we know from the nuclear bombings at Hiroshima and Nagasaki that the cancers due to the most powerful carcinogen of all, large doses of ionizing radiation, take at least two years to begin showing up (leukemias) while most solid cancers don’t show up for around 10 years. Given that the vaccines were only introduced to the general population two years ago, even if the vaccines were as powerful a carcinogen as an ionizing radiation dose from being exposed when a nuclear bomb goes off, it would be only now that we might be beginning to see a glimmer of a cancer signal for leukemias, and even then most people didn’t receive the vaccine until months or even a year later, making too soon
Colleges
- American Athletic
- Atlantic Coast
- Big 12
- Big East
- Big Ten
- Colonial
- Conference USA
- Independents (FBS)
- Junior College
- Mountain West
- Northeast
- Pac-12
- Patriot League
- Pioneer League
- Southeastern
- Sun Belt
- Army
- Charlotte
- East Carolina
- Florida Atlantic
- Memphis
- Navy
- North Texas
- Rice
- South Florida
- Temple
- Tulane
- Tulsa
- UAB
- UTSA
- Boston College
- California
- Clemson
- Duke
- Florida State
- Georgia Tech
- Louisville
- Miami (FL)
- North Carolina
- North Carolina State
- Pittsburgh
- Southern Methodist
- Stanford
- Syracuse
- Virginia
- Virginia Tech
- Wake Forest
- Arizona
- Arizona State
- Baylor
- Brigham Young
- Cincinnati
- Colorado
- Houston
- Iowa State
- Kansas
- Kansas State
- Oklahoma State
- TCU
- Texas Tech
- UCF
- Utah
- West Virginia
- Illinois
- Indiana
- Iowa
- Maryland
- Michigan
- Michigan State
- Minnesota
- Nebraska
- Northwestern
- Ohio State
- Oregon
- Penn State
- Purdue
- Rutgers
- UCLA
- USC
- Washington
- Wisconsin
High Schools
- Illinois HS Sports
- Indiana HS Sports
- Iowa HS Sports
- Kansas HS Sports
- Michigan HS Sports
- Minnesota HS Sports
- Missouri HS Sports
- Nebraska HS Sports
- Oklahoma HS Sports
- Texas HS Hoops
- Texas HS Sports
- Wisconsin HS Sports
- Cincinnati HS Sports
- Delaware
- Maryland HS Sports
- New Jersey HS Hoops
- New Jersey HS Sports
- NYC HS Hoops
- Ohio HS Sports
- Pennsylvania HS Sports
- Virginia HS Sports
- West Virginia HS Sports
ADVERTISEMENT
Two genomics experts on record: mRNA covid 💉 contaminated ☠️
- Thread starter Boston.Knight
- Start date
What a cluster. This is mass genocide, they're not going to be able to sweep this under the rug like in the past 💰🤦♀️☠️
Unsurprisingly, it didn’t take long for antivaxxers to try to link COVID-19 vaccines to cancer as well, with attempts beginning even before the FDA granted an emergency use authorization (EUA) for the Pfizer vaccine two years ago. First, they falsely claimed that the mRNA vaccines “permanently alter your DNA” even though basic molecular biology should have told them that mRNA in the vaccine can’t integrate into your genome, and that the mRNA vaccines were “gene therapy, not vaccines” complete with a conspiracy theory about the CDC having supposedly changed the definition of a vaccine to include them. Next came misrepresenting old studies to claim that mRNA causes cancer. More recently, long-time antivax lawyer Thomas Renz got access to the Defense Medical Epidemiology Database (DMED), a database tracking the health of military personnel, and used it to make claims that are, at best erroneous and at worst intentionally misleading, specifically that COVID-19 vaccines have resulted in an epidemic of cancer in military personnel, including a nearly 900% increase in esophageal cancer and a nearly 500% increase in breast and thyroid cancers since before the military imposed its vaccine mandate. As I explained at the time, the claims were incredible on their face just from a scientific plausibility standpoint given that we know from the nuclear bombings at Hiroshima and Nagasaki that the cancers due to the most powerful carcinogen of all, large doses of ionizing radiation, take at least two years to begin showing up (leukemias) while most solid cancers don’t show up for around 10 years. Given that the vaccines were only introduced to the general population two years ago, even if the vaccines were as powerful a carcinogen as an ionizing radiation dose from being exposed when a nuclear bomb goes off, it would be only now that we might be beginning to see a glimmer of a cancer signal for leukemias, and even then most people didn’t receive the vaccine until months or even a year later, making too soon
Wtf is a turbo cancer?
Over the last several months, antivaxxers have been claiming that COVID-19 vaccines cause “turbo cancer”, cancers (or cancer recurrences) of a particularly aggressive and fast-growing variety diagnosed in younger and younger patients. “Turbo cancer” is not a thing, and the evidence cited is as weak as any antivax “evidence”, including anecdotes and misinterpretation of epidemiology
Over the last several months, antivaxxers have been claiming that COVID-19 vaccines cause “turbo cancer”, cancers (or cancer recurrences) of a particularly aggressive and fast-growing variety diagnosed in younger and younger patients. “Turbo cancer” is not a thing, and the evidence cited is as weak as any antivax “evidence”, including anecdotes and misinterpretation of epidemiology
Cat tweeter and a German. You have to trust them. They sell supplements. Lord Alfred has spoken. Eat paste. Sip silver buy gold. Mass genocide. Italian Venus fly traps.
Ever
I don't think this is accurate. I read something different on Facebook.
What a cluster. This is mass genocide, they're not going to be able to sweep this under the rug like in the past 💰🤦♀️☠️
I don't think this is accurate. I read something different on Facebook.
Antidotally you may be correct.There’s the lord Alfred we know and love. Turbo cancer. Eat paste. Sip silver. Buy gold. Italian Venus fly traps. Check out this tweet from supplement hockers.

FAKE NEWS: Myocarditis-related deaths, linked to anti-COVID vaccination
A study unrecognized by the medical community claims myocarditis, a disease that killed a large number of patients in the last two years, is tied to anti-COVID-19 vaccination.www.veridica.ro
The rate of CNS events and neurological complications these days never existed at rates before 2021 like today, almost entirely young people.
They could never safely scale, then went cheap. A very lethal 1-2 punch. Chopped up the DNA into tiny little bits to scatter like buckshot throughout your body making cancer much worse. Like a murderer chops up a body and throws the pieces into the river hoping they would decompose and disappear. What a cluster. Can't make this sh*t up. 💰 🤦♂️
And here is another expert this time out of Germany that replicated the findings and is on record! Man, this could be the one that takes down this entire house of cards
Yep. The first EU leak was how the EMA allowed Pfizer to ship contaminated vials only because they were to be used on the elderly only. Unfortunately Germany mandated them on everyone healthy.What a cluster. This is mass genocide, they're not going to be able to sweep this under the rug like in the past 💰🤦♀️☠️
It'll take awhile, but it's all coming out in Germany. But at least their Fauci admitted he was wrong starting late last year. His regret is growing as well. But Germany is a country that compensates those harmed by its policies.
Here in the US, it will take a class action lawsuit against the US government, and that will require enough justices to fight the system.
Last edited:
Since you have me on ignore, I guess you won’t mind me sharing with mikes and everyone else all the maniacal Dms you’ve sent me through the years. Cool.Yep. The first EU leak was how the EMA allowed Pfizer to ship contaminated vials only because they were to be used on the elderly only. Unfortunately Germany mandated them on everyone healthy.
It'll take awhile, but it's all coming out in Germany. But at least their Fauci admitted he was wrong straying late last year. His regret is growing as well. But Germany is a country that compensates those harmed by its policies.
Here in the US, it will take a class action lawsuit against the US government, and that will require enough justices to fight the system.

Scans reveal new clues to long Covid symptoms - BBC News
Further evidence emerges that a serious infection can leave some major organs with long-term damage.

Long Covid linked to changes in some organs - study
A third of people hospitalised with Covid-19 have "abnormalities" in multiple organs months after getting infected, according to a UK study, potentially shedding light on the elusive condition of long Covid.
What Is Long COVID?
Many people recover fully within a few days or weeks of being infected with SARS-CoV-2, the virus that causes COVID-19. But others have symptoms that linger for weeks, months, or even years after their initial diagnosis. Some people seem to recover from COVID-19 but then see their symptoms return, or they develop new symptoms within a few months. Even people who had no symptoms when they were infected can develop symptoms later. Either mild or severe COVID-19 can lead to long-lasting symptoms.Long COVID, long-haul COVID, post-COVID-19 conditions, chronic COVID, and post-acute sequelae of SARS-CoV-2 (PASC) are all names for the health problems that some people experience within a few months of a COVID-19 diagnosis. Symptoms of Long COVID may be the same or different than symptoms of COVID-19, and some symptoms are similar to those of myalgic encephalomyelitis/chronic fatigue syndrom (ME/CFS). Long COVID can also trigger other health conditions, such as diabetes or kidney disease.

COVID-19: Long-term effects
Some people continue to experience health problems long after having COVID-19. Understand the possible symptoms and risk factors for post-COVID-19 syndrome.By Mayo Clinic Staff
Most people who get coronavirus disease 2019 (COVID-19) recover within a few weeks. But some people — even those who had mild versions of the disease — might have symptoms that last a long time afterward. These ongoing health problems are sometimes called post-COVID-19syndrome, post-COVID conditions, long COVID-19, long-haul COVID-19, and post acute sequelae of SARS COV-2 infection (PASC).
What is post-COVID-19 syndrome and how common is it?
Post-COVID-19 syndrome involves a variety of new, returning or ongoing symptoms that people experience more than four weeks after getting COVID-19. In some people, post-COVID-19syndrome lasts months or years or causes disability.Research suggests that between one month and one year after having COVID-19, 1 in 5 people ages 18 to 64 has at least one medical condition that might be due to COVID-19. Among people age 65 and older, 1 in 4 has at least one medical condition that might be due to COVID-19.
What are the symptoms of post-COVID-19 syndrome?
The most commonly reported symptoms of post-COVID-19 syndrome include:- Fatigue
- Symptoms that get worse after physical or mental effort
- Fever
- Lung (respiratory) symptoms, including difficulty breathing or shortness of breath and cough
Other possible symptoms include:
- Neurological symptoms or mental health conditions, including difficulty thinking or concentrating, headache, sleep problems, dizziness when you stand, pins-and-needles feeling, loss of smell or taste, and depression or anxiety
- Joint or muscle pain
- Heart symptoms or conditions, including chest pain and fast or pounding heartbeat
- Digestive symptoms, including diarrhea and stomach pain
- Blood clots and blood vessel (vascular) issues, including a blood clot that travels to the lungs from deep veins in the legs and blocks blood flow to the lungs (pulmonary embolism)
- Other symptoms, such as a rash and changes in the menstrual cycle
It's also not clear if post-COVID-19syndrome is new and unique to COVID-19. Some symptoms are similar to those caused by chronic fatigue syndrome and other chronic illnesses that develop after infections. Chronic fatigue syndrome involves extreme fatigue that worsens with physical or mental activity, but doesn't improve with rest.
Why does COVID-19 cause ongoing health problems?
Organ damage could play a role. People who had severe illness with COVID-19might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isn't clear how long these effects might last. The effects also could lead to the development of new conditions, such as diabetes or a heart or nervous system condition.The experience of having severe COVID-19 might be another factor. People with severe symptoms of COVID-19 often need to be treated in a hospital intensive care unit. This can result in extreme weakness and post-traumatic stress disorder, a mental health condition triggered by a terrifying event.
What are the risk factors for post-COVID-19 syndrome?
You might be more likely to have post-COVID-19 syndrome if:- You had severe illness with COVID-19, especially if you were hospitalized or needed intensive care.
- You had certain medical conditions before getting the COVID-19 virus.
- You had a condition affecting your organs and tissues (multisystem inflammatory syndrome) while sick with COVID-19 or afterward.
Post-COVID-19 syndrome also appears to be more common in adults than in children and teens. However, anyone who gets COVID-19 can have long-term effects, including people with no symptoms or mild illness with COVID-19.
What should you do if you have post-COVID-19 syndrome symptoms?
If you're having symptoms of post-COVID-19 syndrome, talk to your health care provider. To prepare for your appointment, write down:- When your symptoms started
- What makes your symptoms worse
- How often you experience symptoms
- How your symptoms affect your activities
Your health care provider might do lab tests, such as a complete blood count or liver function test. You might have other tests or procedures, such as chest X-rays, based on your symptoms. The information you provide and any test results will help your health care provider come up with a treatment plan.
In addition, you might benefit from connecting with others in a support group and sharing resources.
If a German said something, I believe it. They invented beer cheese for gods sake. High order intelligence going on over there in the land of litre beers.
I feel left out and not specialSince you have me on ignore, I guess you won’t mind me sharing with mikes and everyone else all the maniacal Dms you’ve sent me through the years. Cool.
You get maniacal DMs and all I get is a threat to “come over and blow my ****ing brains out!”
It's kinda sad considering we're still pushing a false narrative that IgG-predominant, intramuscular vaccines do much at all, despite all the data even back in 2022, even if you're boosted. We're really at that point that most of the data points at genetics, and the vaccines are doing little-to-nothing about that.

 time.com
time.com
And the bivalent Omicron booster last year ended up being worse than the original booster, which the CDC admitted publicly. And privately, the CDC found it ended up making healthy people worse off than being unvaccinated in many cases.
But the greatest loss has been the integrity of our institutions, as politicians get their way, and the trust in them has been destroyed as a result.

You Can Still Get Long COVID If You're Vaccinated and Boosted
Here's what the latest research says
And the bivalent Omicron booster last year ended up being worse than the original booster, which the CDC admitted publicly. And privately, the CDC found it ended up making healthy people worse off than being unvaccinated in many cases.
But the greatest loss has been the integrity of our institutions, as politicians get their way, and the trust in them has been destroyed as a result.
Yep, @UCFBS is anti-Pharma and a ranting lunatic, not only on COVID vaccines, but drugs as well. There is nothing wrong with them at all. Yeah, about that ...
While you guys were screaming about a 40 year-old, proven safe drug, I was posting all the data on this repurposed flu drug that both BARDA and the US DoD spent 9 figures on, and dropped, warning against it, that it causes DNA damage and virus mutations when used against influenza viruses, while Dr. Fauci was toting it.
Guess what? Uh oh! It happened again!!!
Patents define what we use, not actual effectiveness.

 www.nature.com
www.nature.com
Mainstream coverage, hardly 'conspiracy theorists.'

 www.cnbc.com
www.cnbc.com

 thehill.com
thehill.com
And this isn't the first study or analysis with SARS-CoV-2 (COVID-19) either!

 www.beckershospitalreview.com
www.beckershospitalreview.com
 www.ncbi.nlm.nih.gov
www.ncbi.nlm.nih.gov
But, again, we already knew this, from when it was tested against the flu, and the US DoD spend a good fraction of a billion dollars funding it. And who was behind that recommendation? Dr. Fauci. (Molnupiravir = EIDD-2801)
 www.science.org
www.science.org

 theintercept.com
theintercept.com
But Pharma knows what it's doing. They make the right choices for us all ... right?! BTW, this isn't a Biden v. Trump thing, but literally the problem with the industry. They've both been pushing it as a 'game changer.'
And now we have proof it's not just mutating human DNA, but the SARS-CoV-2 virus too! And this was repeatedly predicted!
While you guys were screaming about a 40 year-old, proven safe drug, I was posting all the data on this repurposed flu drug that both BARDA and the US DoD spent 9 figures on, and dropped, warning against it, that it causes DNA damage and virus mutations when used against influenza viruses, while Dr. Fauci was toting it.
Guess what? Uh oh! It happened again!!!
Patents define what we use, not actual effectiveness.

A molnupiravir-associated mutational signature in global SARS-CoV-2 genomes - Nature
A specific class of long phylogenetic branches, distinguished by a high proportion of G-to-A and C-to-T mutations, are almost exclusively found in sequences from 2022, after molnupiravir treatment was introduced, indicating that molnupiravir treatment can give rise to viable mutagenized viruses.
Mainstream coverage, hardly 'conspiracy theorists.'

Merck Covid drug linked to virus mutations that can spread between people, new study says
There is still no evidence that molnupiravir, sold under the brand name Lagevrio, has produced more transmissible or severe variants of Covid.
Bloomberg - Are you a robot?
www.bloomberg.com

Potential link found between Merck antiviral and mutated COVID strains
A new study published Monday links COVID-19 antiviral created by Merck with new mutations of the virus that have been sequenced around the world. Molnupiravir, known commercially as Lagevrio, is on…
And this isn't the first study or analysis with SARS-CoV-2 (COVID-19) either!

Experts worry Merck COVID-19 pill may give rise to new mutations
A new preprint study found that Merck's COVID-19 pill, Lagevrio (molnupiravir), creates new mutations of the virus in some patients who take the drug, Bloomberg reported Feb. 1.
Oxidative DNA Damage by N4-hydroxycytidine, a Metabolite of the SARS-CoV-2 Antiviral Molnupiravir - PMC
Molnupiravir is an antiviral agent recently used for treating coronavirus disease 2019 (COVID-19). Here, we demonstrate that N4-hydroxycytidine (NHC), a molnupiravir metabolite, treated with cytidine deaminase (CDA) induced Cu(II)-mediated oxidative ...
But, again, we already knew this, from when it was tested against the flu, and the US DoD spend a good fraction of a billion dollars funding it. And who was behind that recommendation? Dr. Fauci. (Molnupiravir = EIDD-2801)
AAAS

Federal Whistleblower Says Boss Pushed Him to Buy Drugs That Hadn’t Been Tested in Humans
Rick Bright’s whistleblower complaint points to the influence of industry over the Trump administration’s coronavirus response.
But Pharma knows what it's doing. They make the right choices for us all ... right?! BTW, this isn't a Biden v. Trump thing, but literally the problem with the industry. They've both been pushing it as a 'game changer.'
And now we have proof it's not just mutating human DNA, but the SARS-CoV-2 virus too! And this was repeatedly predicted!
Last edited:
IT
Stands for "Information Technology," and is pronounced "I.T." It refers to anything related to computing technology, such as networking, hardware, software, the Internet, or the people that work with these technologies. Many companies now have IT departments for managing the computers, networks, and other technical areas of their businesses. IT jobs include computer programming, network administration, computer engineering, Web development, technical support, and many other related occupations. Since we live in the "information age," information technology has become a part of our everyday lives. That gmeans the term "IT," already highly overused, is here to stay.COVID-19: Long-term effects
Some people continue to experience health problems long after having COVID-19. Understand the possible symptoms and risk factors for post-COVID-19 syndrome.By Mayo Clinic Staff
Most people who get coronavirus disease 2019 (COVID-19) recover within a few weeks. But some people — even those who had mild versions of the disease — might have symptoms that last a long time afterward. These ongoing health problems are sometimes called post-COVID-19syndrome, post-COVID conditions, long COVID-19, long-haul COVID-19, and post acute sequelae of SARS COV-2 infection (PASC).
What is post-COVID-19 syndrome and how common is it?
Post-COVID-19 syndrome involves a variety of new, returning or ongoing symptoms that people experience more than four weeks after getting COVID-19. In some people, post-COVID-19syndrome lasts months or years or causes disability.Research suggests that between one month and one year after having COVID-19, 1 in 5 people ages 18 to 64 has at least one medical condition that might be due to COVID-19. Among people age 65 and older, 1 in 4 has at least one medical condition that might be due to COVID-19.
What are the symptoms of post-COVID-19 syndrome?
The most commonly reported symptoms of post-COVID-19 syndrome include:- Fatigue
- Symptoms that get worse after physical or mental effort
- Fever
- Lung (respiratory) symptoms, including difficulty breathing or shortness of breath and cough
Other possible symptoms include:
- Neurological symptoms or mental health conditions, including difficulty thinking or concentrating, headache, sleep problems, dizziness when you stand, pins-and-needles feeling, loss of smell or taste, and depression or anxiety
- Joint or muscle pain
- Heart symptoms or conditions, including chest pain and fast or pounding heartbeat
- Digestive symptoms, including diarrhea and stomach pain
- Blood clots and blood vessel (vascular) issues, including a blood clot that travels to the lungs from deep veins in the legs and blocks blood flow to the lungs (pulmonary embolism)
- Other symptoms, such as a rash and changes in the menstrual cycle
It's also not clear if post-COVID-19syndrome is new and unique to COVID-19. Some symptoms are similar to those caused by chronic fatigue syndrome and other chronic illnesses that develop after infections. Chronic fatigue syndrome involves extreme fatigue that worsens with physical or mental activity, but doesn't improve with rest.
Why does COVID-19 cause ongoing health problems?
Organ damage could play a role. People who had severe illness with COVID-19might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isn't clear how long these effects might last. The effects also could lead to the development of new conditions, such as diabetes or a heart or nervous system condition.The experience of having severe COVID-19 might be another factor. People with severe symptoms of COVID-19 often need to be treated in a hospital intensive care unit. This can result in extreme weakness and post-traumatic stress disorder, a mental health condition triggered by a terrifying event.
What are the risk factors for post-COVID-19 syndrome?
You might be more likely to have post-COVID-19 syndrome if:- You had severe illness with COVID-19, especially if you were hospitalized or needed intensive care.
- You had certain medical conditions before getting the COVID-19 virus.
- You had a condition affecting your organs and tissues (multisystem inflammatory syndrome) while sick with COVID-19 or afterward.
Post-COVID-19 syndrome also appears to be more common in adults than in children and teens. However, anyone who gets COVID-19 can have long-term effects, including people with no symptoms or mild illness with COVID-19.
What should you do if you have post-COVID-19 syndrome symptoms?
If you're having symptoms of post-COVID-19 syndrome, talk to your health care provider. To prepare for your appointment, write down:- When your symptoms started
- What makes your symptoms worse
- How often you experience symptoms
- How your symptoms affect your activities
Your health care provider might do lab tests, such as a complete blood count or liver function test. You might have other tests or procedures, such as chest X-rays, based on your symptoms. The information you provide and any test results will help your health care provider come up with a treatment plan.
In addition, you might benefit from connecting with others in a support group and sharing resources.
COVID-19: Long-term effects
Some people continue to experience health problems long after having COVID-19. Understand the possible symptoms and risk factors for post-COVID-19 syndrome.By Mayo Clinic Staff
Most people who get coronavirus disease 2019 (COVID-19) recover within a few weeks. But some people — even those who had mild versions of the disease — might have symptoms that last a long time afterward. These ongoing health problems are sometimes called post-COVID-19syndrome, post-COVID conditions, long COVID-19, long-haul COVID-19, and post acute sequelae of SARS COV-2 infection (PASC).
What is post-COVID-19 syndrome and how common is it?
Post-COVID-19 syndrome involves a variety of new, returning or ongoing symptoms that people experience more than four weeks after getting COVID-19. In some people, post-COVID-19syndrome lasts months or years or causes disability.Research suggests that between one month and one year after having COVID-19, 1 in 5 people ages 18 to 64 has at least one medical condition that might be due to COVID-19. Among people age 65 and older, 1 in 4 has at least one medical condition that might be due to COVID-19.
What are the symptoms of post-COVID-19 syndrome?
The most commonly reported symptoms of post-COVID-19 syndrome include:- Fatigue
- Symptoms that get worse after physical or mental effort
- Fever
- Lung (respiratory) symptoms, including difficulty breathing or shortness of breath and cough
Other possible symptoms include:
- Neurological symptoms or mental health conditions, including difficulty thinking or concentrating, headache, sleep problems, dizziness when you stand, pins-and-needles feeling, loss of smell or taste, and depression or anxiety
- Joint or muscle pain
- Heart symptoms or conditions, including chest pain and fast or pounding heartbeat
- Digestive symptoms, including diarrhea and stomach pain
- Blood clots and blood vessel (vascular) issues, including a blood clot that travels to the lungs from deep veins in the legs and blocks blood flow to the lungs (pulmonary embolism)
- Other symptoms, such as a rash and changes in the menstrual cycle
It's also not clear if post-COVID-19syndrome is new and unique to COVID-19. Some symptoms are similar to those caused by chronic fatigue syndrome and other chronic illnesses that develop after infections. Chronic fatigue syndrome involves extreme fatigue that worsens with physical or mental activity, but doesn't improve with rest.
Why does COVID-19 cause ongoing health problems?
Organ damage could play a role. People who had severe illness with COVID-19might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isn't clear how long these effects might last. The effects also could lead to the development of new conditions, such as diabetes or a heart or nervous system condition.The experience of having severe COVID-19 might be another factor. People with severe symptoms of COVID-19 often need to be treated in a hospital intensive care unit. This can result in extreme weakness and post-traumatic stress disorder, a mental health condition triggered by a terrifying event.
What are the risk factors for post-COVID-19 syndrome?
You might be more likely to have post-COVID-19 syndrome if:- You had severe illness with COVID-19, especially if you were hospitalized or needed intensive care.
- You had certain medical conditions before getting the COVID-19 virus.
- You had a condition affecting your organs and tissues (multisystem inflammatory syndrome) while sick with COVID-19 or afterward.
Post-COVID-19 syndrome also appears to be more common in adults than in children and teens. However, anyone who gets COVID-19 can have long-term effects, including people with no symptoms or mild illness with COVID-19.
What should you do if you have post-COVID-19 syndrome symptoms?
If you're having symptoms of post-COVID-19 syndrome, talk to your health care provider. To prepare for your appointment, write down:- When your symptoms started
- What makes your symptoms worse
- How often you experience symptoms
- How your symptoms affect your activities
Your health care provider might do lab tests, such as a complete blood count or liver function test. You might have other tests or procedures, such as chest X-rays, based on your symptoms. The information you provide and any test results will help your health care provider come up with a treatment plan.
In addition, you might benefit from connecting with others in a support group and sharing resources.
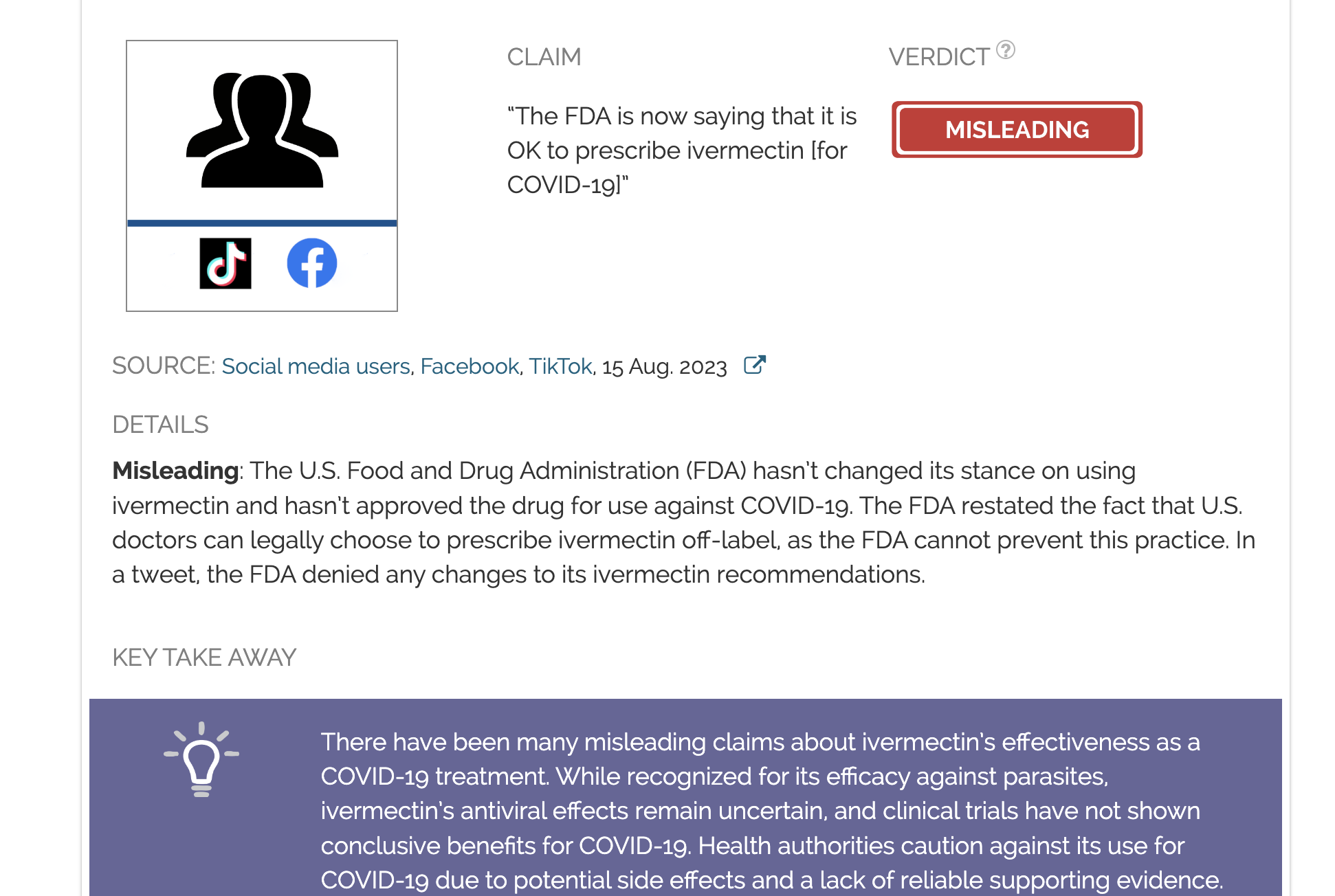
The FDA continues to recommend against ivermectin for treating or preventing COVID-19, despite claims to the contrary
There have been many misleading claims about ivermectin’s effectiveness as a COVID-19 treatment. While recognized for its efficacy against parasites, ivermectin’s antiviral effects remain uncertain, and clinical trials have not shown conclusive benefits for COVID-19. Health authorities caution...

COVID-19 Vaccines, Prior Infection Reduce Transmission of Omicron
California prisons saw more than 20,000 COVID-19 Omicron cases over a five-month period. However, vaccination and boosting kept hospitalization and death rates low.
They also invented this wonderfully accurate numbering system to track people during ww2. They even used that system to provide housing and free burial after death.If a German said something, I believe it. They invented beer cheese for gods sake. High order intelligence going on over there in the land of litre beers.
People also ask
What is the difference between an anecdote and an antidote?
An anecdote is a brief story, usually told because it is relevant to the subject at hand. An antidote is the cure for a poison, but can also be used figuratively for anything that solves a problem. How'd we come up with this antidote?
What is the difference between an anecdote and an antidote?
An anecdote is a brief story, usually told because it is relevant to the subject at hand. An antidote is the cure for a poison, but can also be used figuratively for anything that solves a problem. How'd we come up with this antidote?
So, do we want to honor your father’s do-not-resuscitate order or not?
Probably still not interested?If it’s not a German I’m not interested.
Onkologe: „Ich habe noch nie erlebt, dass sich Krebserkrankungen so verhalten“
Junge Menschen in den Zwanzigern, Dreißigern und Vierzigern entwickeln aggressive und schnell wachsende „Turbokrebserkrankungen“.
„Der jüngste Fall, den ich gemeldet habe, war ein zwölfjähriger Junge, der einen Moderna-Impfstoff erhalten hatte. Vier Monate später erkrankte [er] an Hirnkrebs im vierten Stadium. Und sechs Monate später starb er“, berichtete er
@MakisMD
„Ich habe in meiner Karriere wahrscheinlich 20.000 Krebspatienten diagnostiziert. Ich habe noch nie erlebt, dass sich Krebs so verhält.“
Nobody has an immune system like Igor Chudoff and Lord Alfred. With their powers combined they will warn the world about the terrors of vaccination and the wonders of silver, gold, and paste.
Be honest: you cut yourself when you floss, don’t you?
ADVERTISEMENT